The deteriorating patient: a 'chain of survival' approach to improving outcomes
Thinking about the whole patient journey may help outcomes in acute deterioration
Long ago, I was a newly-minted junior doctor working on the surgical ward of a big, tertiary-care hospital. (If that term ‘tertiary care’ is unfamiliar to you, substitute the word ‘scary’).
Tertiary care is where the sickest and most complex patients go when smaller hospitals can’t fix them. As a patient, you never want to need a tertiary hospital.
Back then, my patients were particularly sick. My team did a lot of Whipple's operations and other partial pancreatic resections. Once again, as a patient, you also never want to need either of these operations.
When on call, I was only doctor that covered the main wards during the night. Just out of medical school, lacking both confidence and clinical skill, I was out of my depth for much of the time.
During my six months stint on this ward, the phrase ‘deteriorating patient’, took on a a particularly terrifying meaning. I was often the last medically qualified person between a patient’s rapid drop in blood pressure and what in the US is euphemistically called ‘failure to rescue’.
[Note: I write this as the 10th UK strike of doctors-in-training has begun, which makes me think this is appropriate subject. I’m not certain how much things have improved for such junior doctors covering wards at night, but my hunch is that fewer, poorer qualified and less motivated doctors won’t improve patient outcomes.]
Fast forward a few decades and last week I was presenting at a webinar to a group of hospital leaders about how to recognise, manage and - above all - improve the outcomes for ‘the deteriorating patient’.
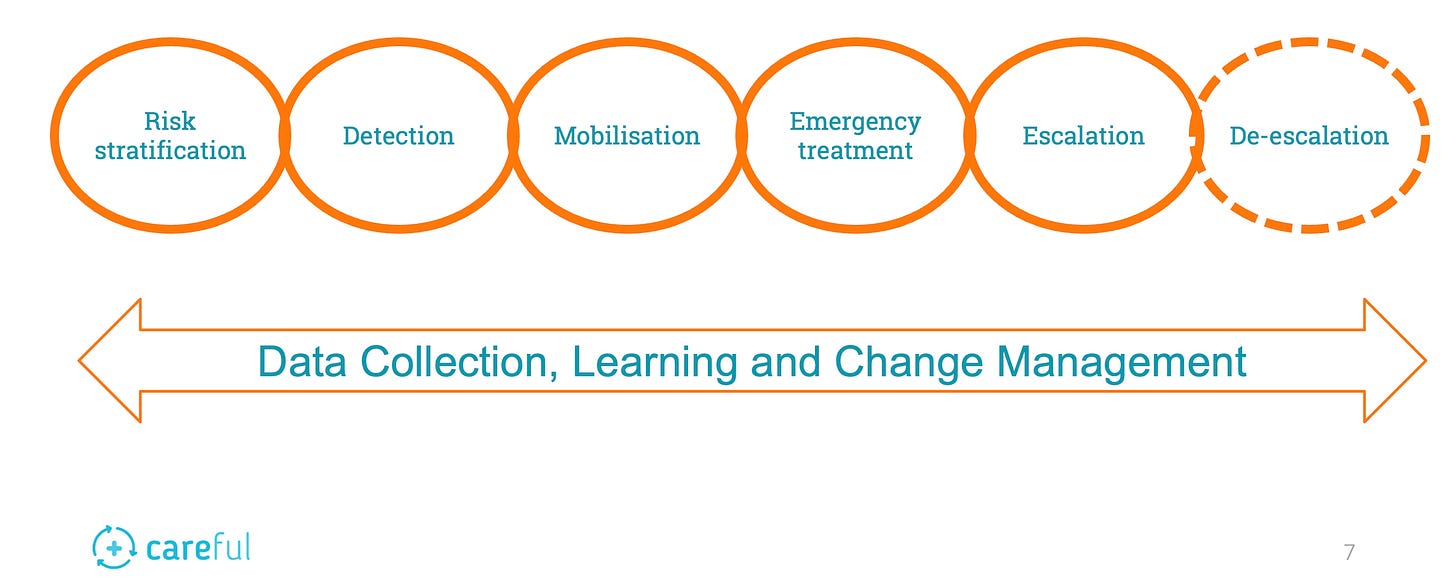
To give structure to the conversation, I concocted a 'chain of survival' concept using a type of diagram that is often used when talking about resuscitation and CPR.
This is my ‘deteriorating patient chain of survival’
What follows is a few thoughts and questions that might guide hospital leaders trying to implement improvements in this difficult area of operational and clinical practice.
Full disclosure: the author is CEO of CAREFUL - which has developed a care coordination platform that addresses many of the problems identified in this blog
Risk Stratification
Who is most likely to deteriorate?
Identifying which patients are most at risk is key to preventing deterioration. Individual patients, and groups, need to be flagged, treated and monitored appropriately.
Questions worth asking:
Where are your patients most at-risk of deterioration? (Hint: don’t forget the ED and radiology).
Who is looking after them (and what are the staff’s competencies)?
What can you do to reduce the risks or improve earlier detection?
Can these patients be pre-optimised (e.g. through sepsis pathways or pre-loading CT-contrast patients with fluid?)
Detection
Is this being done correctly?
Detection through track-and-trigger has received most attention over the last few years - notably through NEWS2 in the UK .
Remember that NICE guidance suggests that other measures may be appropriate. Pain scores may be important, especially in children.
Is it being done at all?
Have staff really been trained and have you signed off their competencies
Doctors and AHPs may need training in detection
Are you overly reliant on these systems? Is there scope for clinical ‘gestalt’.
Mobilisation
If you ask them, will they come?
Assuring the rapid response to a trigger can be difficult; surgeons may be in theatre, juniors are overwhelmed with tasks on other wards; deteriorations my happen simultaneously.
A ‘peri-arrest’ system that mobilises the crash team before a patient hits rock-bottom is often very useful. And of course, having dedicated outreach teams is effective but resource intensive
How well do your mechanisms of notification work? Bleeps, crash-calls, message?
What is the likely availability of team members (“Sorry she’s in theatre” was a phrase I dreaded as a new doctor)
Dedicated teams are likely best, but they are costly
Emergency Treatment
Can the emergency team do what is needed?
If you mange to get the team to the patient’s bedside in time, the question is what is then possible? Do they have both the capabilities and resources to rescue the patient?
Where are your crash carts?
Are they stocked and checked?
What drugs are immediately availability?
Does your emergency transfusion protocol produce blood quickly enough?
What are the advanced life support capabilities of your team?
This part has been the focus of much resuscitative and acute life-support training for years, so many of these answers will seem self evident. It’s worth reviewing them nonetheless.
Escalation
Who is going to take over?
Once you’ve stabilised the patient, they are unlikely to stay in the same location. Many will need enhanced care (either HDU or ICU). Do you have enough beds? I can almost guarantee the answer is no. And do you have the staff and resources to make the transfer?
Are your escalation pathways, procedures and decision-making documented and clear?
Who makes the decision, who else do you need to involve?
What is the relationship with other providers e.g. tertiary care centres? Are they easily contactable (eg via negotiated ‘green lanes’)
Do you have a guaranteed service-level agreed for ambulance transfers?
This stuff gets complicated. It needs to be documented - and ideally practiced in simulation.
De-escalation
Will they survive the return to the ward?
Assuming the patient survives the escalation of care, you need to consider the risks of de-escalation. I was told of one patient who died on the ward from sepsis following a return from ICU because the antibiotic regime was misunderstood or mislaid.
Who decides when the patient is ready? (Remember ICU is always full)
How do you communicate the care plan to the ward?
How do you monitor these patients (return to step 1, Risk Stratification).
When do you make the transfer? (The evidence says that patients do badly if they are transferred during the night)
Change management
How do you keep changing and improving?
The biggest challenge overall is working out how to make the necessary incremental changes to the processes and systems described above.
How do you collect the data for audits/continuous improvement?
What are the standards you set?
How do you define success?
Who has accountability for this?
What are your change management and governance structures?
Recognising and managing a deteriorating patient throughout their stay requires complex change management and governance. It is a multifaceted challenge that requires a coordinated approach.
Ideally, this should be implemented by a focused multidisciplinary team, with senior clinical and operational membership. Data needs to be collected, analysed and changes made to training, competency development, processes and communication systems.
Without that, you risk keeping putting junior staff in the invidious position of being the ones at the bedside during a ‘failure to rescue’.
Some useful evidential links
NEWS2 https://www.england.nhs.uk/ourwork/clinical-policy/sepsis/nationalearlywarningscore/
NICE Clinical Guidance CG 50 (25-Jul-2007) Acutely ill adults in hospital: recognising and responding to deterioration https://www.nice.org.uk/guidance/cg50/chapter/Recommendations#identifying-patients-whose- clinical-condition-is-deteriorating-or-is-at-risk-of-deterioration
Safe system framework for children at risk of deterioration https://www.rcpch.ac.uk/resources/safe-system-framework-children-risk-deterioration
Hall KK, Lim A, Gale B. Failure To Rescue. In: Hall KK, Shoemaker-Hunt S, Hoffman L, et al. Making Healthcare Safer III: A Critical Analysis of Existing and Emerging Patient Safety Practices [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2020 Mar. 2. Available from: https://www.ncbi.nlm.nih.gov/books/NBK555513/